Diabetic foot care is of critical importance for many diabetics. Diabetes comes in many forms and levels of severity. The most dire consequences stem from diabetes that goes undiagnosed for extended periods of time. Blood sugars gradually elevate as the body builds a tolerance to the increased blood sugars. Blood sugars can become very high 300+, when this happens, these elevated blood sugars do permanent damage to the large and small blood vessels, organs of the body, nerves, immune system, among others.

Vascular/pressure ulcer L great toe.
Peripheral Vascular Disease
Blood vessels both large and small can be affected by extended periods of elevated blood sugars. These vessels can become occluded decreasing blood blow to the extremities. Reduced blood flow leads to ulcerations, ischemia, pain, infection and potentially amputation. Treatment can include bypass surgery, stints, angioplasty, or other methods of opening vessels.
- Dry Gangrene Finger (2)
- Dry Gangrene Finger Image 2
- Auto amputation of the finger
- Borderline gangrene
- Vascular wounds of the feet
- Dry Gangrene Vascular Wound
- Vascular/pressure ulcer L great toe.
- Dry Gangrene Toe
Peripheral Neuropathy

Extended periods of elevated blood sugars can cause permanent damage to nerves of the extremities. These nerves are critical for many feedback loops with the brain and sensation. These nerves are responsible for hot/cold, pain, moisture control in the skin, proprioception, 2 point discrimination, and sensation. Proprioception is knowing where your joints are in their range of motion i.e. toe up or down, etc.
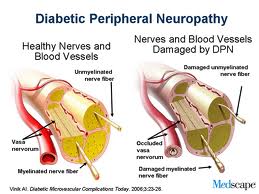
Neuropathy progresses differently for each individual. The most common progression of peripheral neuropathy starts with an increase in sensitivity (hypersensitivity), burning, tingling (parethesias), then progresses to a point of total numbness and a total lack of all feed back loops.
Each of these stages has its own potential problems. The initial stages involving hypersensitivity and parethesias can be very uncomfortable to a point of limiting ones ability to cope with the pain, loss of sleep, and decrease quality of life. This stage can be treated by one of a few medications available on the market. Lyrica and Neurotin are 2 of the most commonly prescribed medications currently. Both can be very effective, however often require close monitoring of the dosages, because side effects are common.
Latter stages of peripheral neuropathy can be devastating if the feet are not closely monitored. When the feet become numb and the feed back loops are no longer functioning properly, it is easy for injuries and infections to go undetected. It is not uncommon for diabetics to show up in the office with a puncture wound, abscess, joint atrophy (Charcot joint), ulceration, or infection and not have any pain or knowledge of a problem. This is the most common cause of amputation in diabetics.
Decreased Ability to Fight Infection (Immunopathy)
With diabetes comes the decreased ability to fight infections, this can be due to lack of circulation. The circulation is responsible for not only delivering red blood cells (RBC’s) but also white blood cells (WBC’s), there many different types of WBC’s, if they are not getting to the extremities the risk of infection increases.
Diabetic Foot Care
With everything above it now becomes more obvious why diabetic foot care is so important. Here is what we need our diabetic patients to do:
- Monitor blood sugars, diet, and exercise appropriately for your health conditions.
- Look at your feet daily, use a non-glass mirror to inspect the bottom of your feet. If you have diabetic retinopathy have a friend or nurse look at your feet regularly.
- Wear white socks when possible, not because they are the most stylish – because bleeding and other drainage are easy to see,.
- If anything looks differently, do not wait, call your podiatrist, yes you need a podiatrist on speed dial.
- Make regular visits to a podiatrist for examinations, at least every 6 months, more often for palliative foot care if you are suffering from complications of diabetes in your feet.