Heel Pain
Heel Pain
Plantar Fasciitis
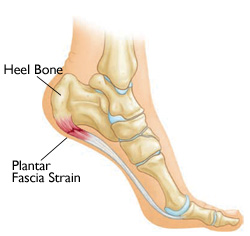
The most common cause of heel pain, plantar fasciitis is characterized by pain in the heel after rest (poststatic dyskinesia) then decreasing slowly with exercise. The plantar fascia is a ligament extending from the calcaneus to the metatarsal heads of the foot. Plantar fasciitis is inflammation of the plantar fascia ligament, most commonly as it attaches to the heel bone (calcaneus), but it can be anywhere along the plantar fascia.
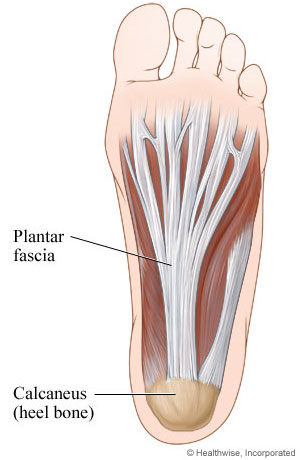
Plantar Fascia inflammation is the most common cause of heel pain.
This inflammation worsens with periods of relaxation as the ligament is allowed to relax. When the foot is loaded by standing the ligament is stretched and areas of inflammation along the ligament become very painful. This pain can follow the plantar fascia into the arch, but is usually isolated to the heel. The plantar fascia becomes inflamed from repeated twisting or torqueing of the ligament due to an unstable foot.
How common is plantar fascitis?
Plantar fasciitis is an important public health disorder as it is the most common cause of heel pain in the outpatient setting.1 Ten percent of people in the United States may present with heel pain over the course of their lives, with 83% of these patients being active working adults between the ages of 25 and 65 years old.3,4 Two large national data sets of ambulatory care data (excluding visits to podiatrists or federal, military, or Veterans Administrations facilities) from the Centers for Disease Control and Prevention’s National Center for Health Statistics found that plantar fasciitis accounts for an average of one million patient visits per year to medical doctors.4 Sixty-two percent of these visits were made to general medicine clinics, while 31% of patients were evaluated by orthopaedic or general surgeons. Additionally, a recent survey of members of the American Podiatric Medical Association revealed that plantar fasciitis/heel pain was the most prevalent condition being treated in podiatric clinics.19 Within the current literature, prevalence rates of plantar fasciitis among a population of runners have been shown to be between 4% and 22%.20,21
Rano et al11 found that the average age of the patients presenting to their facility with heel pain was almost 10 years higher than controls who presented for other reasons. Matheson et al’s retrospective review of 1407 patients from an outpatient sports medicine clinic, found that younger athletes had a lower prevalence of plantar fasciitis (2.5%) than older athletes (6.6%).17 The association of plantar fasciitis with increasing age is consistent with the histopathological findings of degenerative, rather than inflammatory, changes within the plantar fascia.2 These degenerative findings support the hypothesis that plantar fasciitis is secondary to repetitive microtrauma caused by prolonged weightbearing activities.13 The constant overload inhibits the normal repair process, resulting in collagen degeneration, which causes both structural changes and perifascial edema.15,22 These changes in turn lead to a thicker heel pad, which has been shown to be associated with pain in individuals with plantar fasciitis.12,13 Increasing heel pad thickness leads to a loss of heel pad elasticity; both of these factors are associated with increasing age and increasing BMI.23 The decrease in elasticity of the fascia seen with increasing age is associated with a decrease in shock absorbing capabilities,23 which may be a result of the degenerative fascia’s inability to resist normal tensile loads.22 It is this decrease in shock absorbing capability that is believed to cause the pain associated with plantar fasciitis.
Nerve Entrapments and Heel Pain
There are various nerves in the foot that can malfunction when they experience abnormal pressure. There are nerves in the heel area that can cause heel pain when entrapped and irritated by muscle and ligament. This pain is different than the pain experienced by plantar fasciitis and is most commonly characterized by burning, tingling, or the feeling of pins and needles being stuck into their feet.
Injections of steroids can be effective at limiting the inflammation around the nerve, ligaments, scar tissue, or other structures entrapping the nerve. Orthotics can sometimes relieve some of the stress on the nerve by changing the biomechanics of the foot and reducing stress along the areas of entrapment.
Surgical resection of the impinging tissue may be required. These procedures depend on the nerve, location, and impinging structure.
Stone bruise of the Heel and Calluses
Occasionally, a bruise or callus can develop under the heel bone or calcaneus. I am grouping these two together because calluses directly under the calcaneus will sometimes cause bruises. Bruises or contusions are nothing more than inflammation of the soft tissues and the pain is often characterized as dull and achy. This pain does not go away or decrease with exercise as it does with plantar fasciitis. Inflammation under a normal weight bearing surface causes pain. This contusions can be caused by many different problems associated with an individuals foot. The more common causes are lack of fat pad under the heel, traumatic injury, over doing it, and poor shoe gear.
Treatment corresponds to the causative factor. Treatments that work include gel heel pads or insoles, debriding a callus (if one exist), icing, rest, and better shoe gear.
Traumatic Heel Injury
Traumatic injury to the heel other than that causing a bruise or contusion of the soft tissue around the heel would be a fracture of the calcaneus or dislocation of the surrounding joints. Calcaneal fractures and dislocations of joints in the foot are medical emergencies and require an ER visit. These injuries may require surgery or in some cases can be reduced put back in place without surgery. In either case, it will depend on the experience of the physician on call.
Ulcers and wounds of the heel are visible but may have more going on that one would expect. These are most commonly seen in patients with peripheral arterial disease (PAD) (PVD), Peripheral Neuropathy (PN), and/or people limited to bed. Wounds of the heel depending on the location can take months or even years to heel if they heel at all. It is important treat the cause of the ulcer and make sure the ulcer is clean. As I tell my patients there are certain factors required to heel this wounds these factors include:
- Adequate blood supply
- Good nutrition
- No infection
- Reduction in or no pressure to the area
If these factors are able to be accomplished a wound can and usually will heal no matter what topical is used.
Heel Pain and Arthritis
Arthritis or degeneration of the joints in the rear foot can cause various pains in and around the joints involved. Degeneration of joints is a normal breakdown of cartilage responsible for cushioning and maintaining lubrication of our moving “bony hinges.” There are many factors which can expedite this degeneration including, genetics, obesity, unstable feet, fractures involving the joints, misaligned joints among other things. Pains are usually described as dull, achy, stiffness, and sometimes have post-static dyskinesia (pain after rest.)
Conservative treatments include orthotics, steroid injections, NSAID’s, and supplements to aid in lubrication. Orthotics are used to help stabilize the foot and reduce motion of the joints involved. With the increased stability and reduction in joint motion there is often a significant reduction in the pain. It is important to understand none of the conservative or surgical treatments are able to undo the damage that has been done. In all cases we are treating the symptoms. Steroids are potent anti-inflammatories and can reduce acute inflammation associated with flare ups. NSAIDS or Non-Steroidal Anti-Inflammatories can be used to reduce pain as needed. As stated earlier consult your doctor if you have a history of any bleeding problems including but not limited to gastric ulcers, people on Coumadin, or hemophiliacs. Supplements like glucosamine and chondroitin have been shown to reduce further damage of the joints.
The surgical treatments for arthritis in the area of the heels often result in fusions of the joints involved. This can require multiple fusions if there are more than one joint involved. A fusion is a permanent locking of the joint by removing the joint and placing screws or other souses of fixation to stabilize the bones and allow the bones to heel. If there is no motion there is no pain due to arthritis. Fusions stopping the motion in one or more joints causes an increase in the need for motion in other joints. As one can imagine this can cause other problems and chronic pain. The success rate for these procedures varies greatly from patient to patient and often depends on how much pain the patient had prior to surgery.